In this article Dr Andrew provides a review of the current understanding of sudden unexplained infant death (SUID) including SIDS, a term rapidly falling out of common usage and the positive affect of the American Academy of Pediatrics’ “Back to Sleep” program.
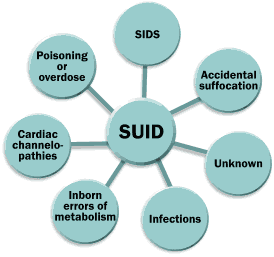
SUID occurs in previously healthy babies, suddenly (typically during sleep) and without obvious or explainable cause, even after a death scene investigation and autopsy have been carried out.
Definition and Rates of SUID Occurrence
The original definition of what was then known as Sudden Infant Death Syndrome (SIDS) was as follows: “The sudden death of an infant under one year of age which remains unexplained after the performance of a complete postmortem investigation, including an autopsy, an examination of the scene of death, and a review of the case history.” Per National Institute of Child Health and Human Development Consensus Statement – 1989.
“SIDS” is but one potential cause Others include accidental suffocation, infections, genetic defects and occult homicidal violence.
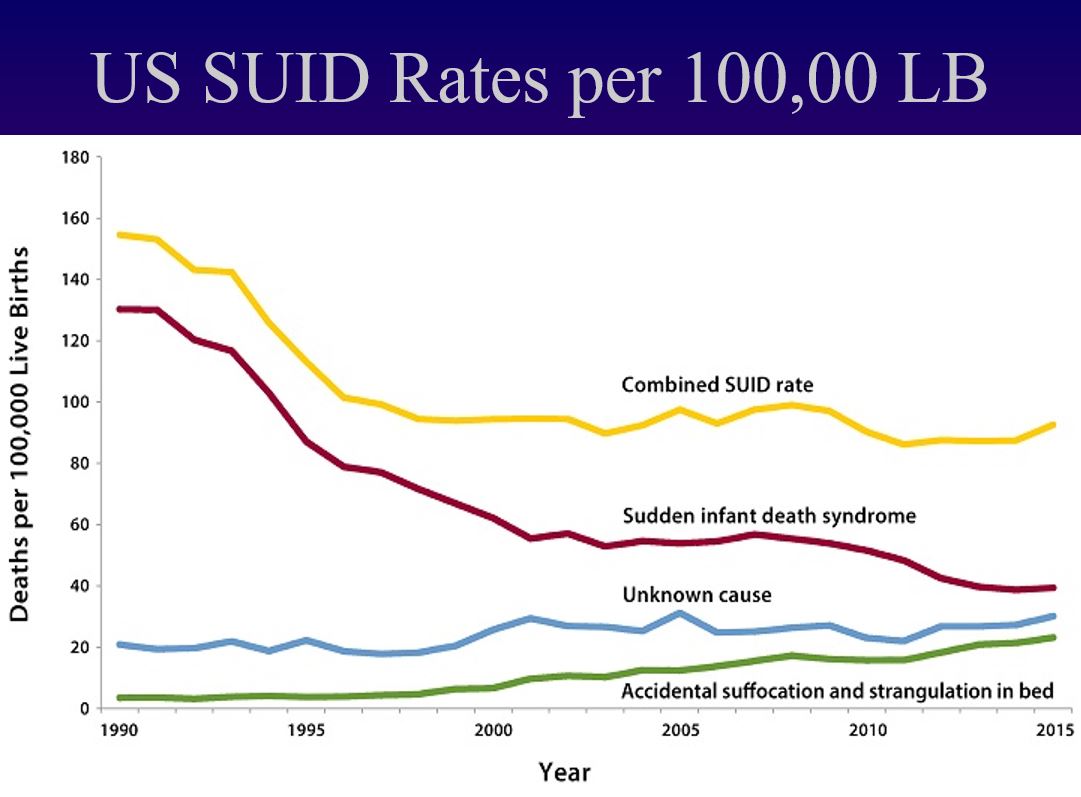
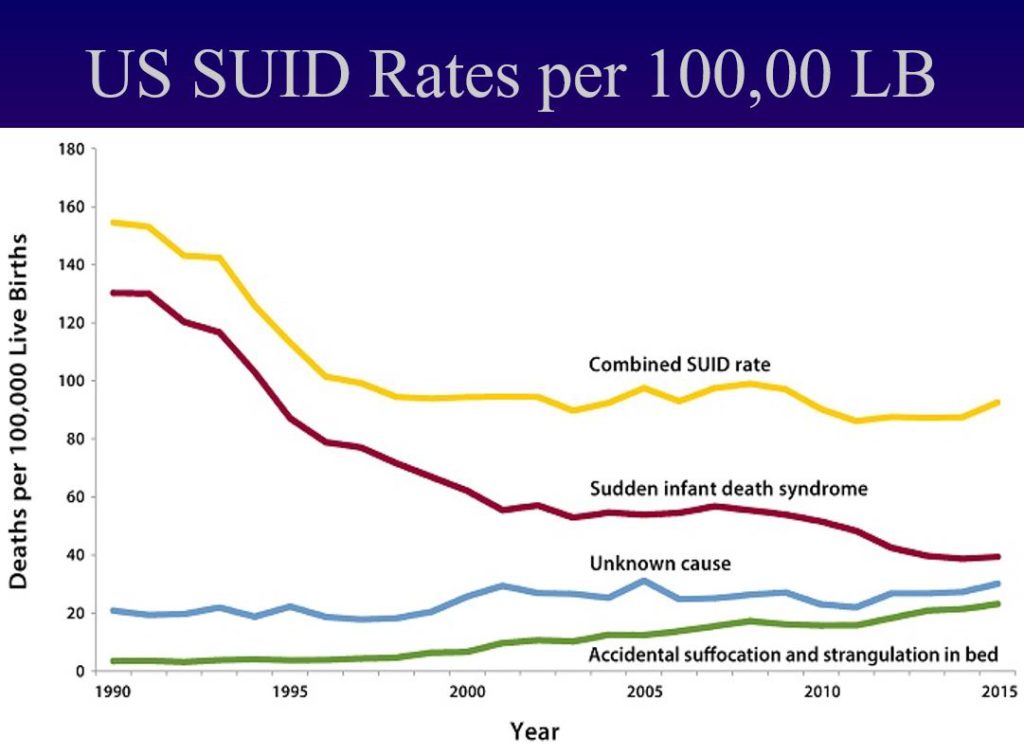
There has been a diagnostic shift in death certification, with some medical examiners referring to fewer deaths as SIDS and more as accidental suffocation or unknown. This is reflected in the article cited :
Mitchell, Krous, Donald and Byard, Changing Trends in the Diagnosis of Sudden Infant Death, Am J Forensic Med and Pathology; 21(4): 311-314, 2000 – noted Increases in diagnoses of accidental asphyxia due to unsafe sleeping environments
A 2004 Consensus Conference in San Diego resulted in a refined definition of SIDS:.
Sudden, unexpected death of an infant less than one year of age, with onset of the fatal episode apparently occurring during sleep, that remains unexplained after a thorough investigation, including performance of a complete autopsy and review of the circumstances of death and the clinical history.
The reader will note the only refinement is the addition of the clause regarding sleep.
Seeking a more stratified approach to classifying the variations presented by SUID in actual practice, a formal classification system was proposed:
Category IA SIDS: Classic features and complete documentation
Category IB SIDS: Classic features but incomplete documentation
Category II SIDS: Meet category I criteria with specific exceptions
Unclassified Sudden Infant Death: Does not meet category I or II criteria, alternative diagnoses of natural or unnatural conditions are equivocal, including cases in which autopsy is not performed
This never gained traction among medical examiners and coroner’s and is not in current use.
This writer, with colleagues from the CDC made yet another attempt at developing a classification system, but it likewise has failed to be widely adopted by those who certify SUID:
Shapiro-Mendoza, CK, Camperlengo, L, Ludvigsen, R, Cottengim, C, Anderson, RN, Andrew, T, Covington,T, Hauck, FR, Kemp, J, MacDorman, M.Classification System for the Sudden Unexpected Infant Death Case Registry and its Application. Pediatrics; originally published online June 9, 2014; DOI: 10.1542/peds.2014-0180.
Regardless of how such deaths are coded, many Child Death Review teams review SUID/SIDS deaths because with the specific aim of developing prevention strategies.
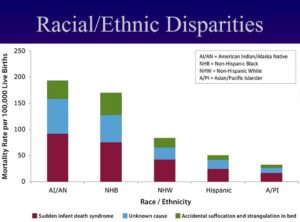
Racial/Ethnic Disparities have been noted:
The following are considered additional SUID Risk Factors – Note: risk factors and causes are two very different concepts
- Racial, ethnic, socioeconomic
- Maternal age
- Lack of prenatal care
- Nutrition
- Infection
- Anemia
- Maternal substance abuse
- Tobacco
- Alcohol
- Other drugs
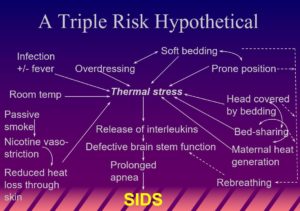
SIDS “Triple Risk Model” – (adapted from Filiano and Kinney)
Introduced in 1994, but still relevant today is concept of the “perfect storm” of a uniquely vulnerable infant at a critical stage of neurodevelopment being physiologically challenged by environmental circumstances initiating the lethal train of events terminating in “SIDS.”
Considered as a subset of SUID, “SIDS,” also known as cot death or crib death, typically occurs between the hours of 00:00 and 09:00. There is usually no evidence of struggle and no noise produced. It cannot be overemphasized that the exact cause of SIDS is unknown. The triple risk model suggests that a combination of factors a specific underlying infant susceptibility, a specific time in development, and an environmental stressor provides the fatal substrate for death to ensue.
In this hypothetical, the combination of infection with low grade fever, soft bedding, prone sleep position, bed-sharing, maternal smoking and bedding result in heat stress and disruption of brain stem function in a vulnerable infant who succumbs to SIDS.
It is likely that genetics plays a role in SIDS, and this is a focus of much of current research.
It is also important to note that there has never been any credible evidence that vaccines are a root cause of these deaths
Sudden infant death Investigative time line
- Event discovery
- Notification of first responders (EMS/FD/PD)
- Attempted resuscitation?
- Transport to emergency room?
- Notification of Medical Examiner
- Investigation
- Scene Investigation
- Basic demographics
- Circumstances of discovery
- Precise location and position of infant when last seen alive vs. when body discovered
- Clothing, bedding
- Last feeding
- Actions taken on discovery
- Environmental factors
- Autopsy
- Follow-up
- Scene Investigation
Sleep Position
Sleeping prone (on the back) has been found to reduce the risk of SIDS, and as a result, this position is recommended by the AAP. In 1994 a “Back to Sleep” campaign was launched and is credited with the reduction in SIDS deaths:
- SIDS rate falls from 1.416/1000 LB to 1.3 between 1985 and 1991
- AAP Statement on sleep position, 1992
- SIDS rate falls from 1.3 to 1.03 in 1994
- “Back-to-sleep” campaign launched 1994; subsequently renamed “Safe to Sleep”
- Percentage of infants less than 8 months of age put down for sleep in supine or lateral position increases from 28% in 1992 to 78% in 1997
- SIDS rate tumbles from 1.03 to 0.69 by 1997
Rachel Moon and The Daycare Bombshell
- Moon, a pediatrician at Children’s Hospital in Washington, D.C. published a retrospective study of 1,916 SIDS cases
- 4% of deaths occurred in child care vs. a 7% rate predicted by time spent by infants in out of home child care
- 60% of these were in non-commercial settings
- Infants in child care were more likely to be last placed or found prone, particularly when the usual sleep position was side or supine.
The more things change . . . The volatile issue of prone versus supine sleep for infants:
- Council of Salisbury, 1217 – “Priests were enjoined to warn women . . . about securing them Infants in their cradles in such a way that they could not turn over on their faces.”
- 1908 anticipatory guidance manual for infant care recommended a supine (face up) sleep position
- 1944 – Abramson sounds an alarm regarding the risks of prone sleep
- 1946 – The Common Sense Book of Baby and Child Care by Benjamin Spock endorsed supine sleep
- 1957 – Spock recommends prone sleep in his second edition on the theory that infants were less fussy and less inclined to aspirate in this sleep position
- 1958-1987 – Link between prone sleep and SIDS noted
- 1972, 1979 and 1985 – Spock holds firm to his prone sleep recommendation in subsequent editions.
- 1977 – Babyhood by Penelope Leach also recommended the prone position for sleep for the same reasons as Spock
- Kemp and Thach publish their re-breathing hypothesis in 1991 – using an animal model they showed that re-breathing expired air in the face down position could lead to the build-up of CO2 and decreased respiratory drive
- Currgenven, made this very same observation over a century earlier, in1871 – “The bed clothes at the same time covering its head; (the baby) dies without a struggle suffocated by carbonic acid exhaled from its own lung”
Infants in Adult Beds
There is vigorous debate over the wisdom of allowing babies to share their parents’ bed.
Studies suggest this practice remains on the rise, increasing from 5.5 to 12.8% between 1993 and 2000. African-Americans were 4 times as likely as Caucasians; Asians, 3 times as likely.
Bed-sharing infants were 2 times as likely to be covered by a quilt or comforter. Nearly 50% of low-income, inner city mothers reported bed-sharing in the first year.
Proponents of bed sharing argue that it is beneficial allowing for more and longer breast feeding. There are also claims that it is “protective” against SIDS.
“Although the prevention of overlay deaths is an appropriate and worthwhile goal, the unconditional implication that (co-sleeping) is harmful is inappropriate, untrue and not supported by scientific research.” – James J. McKenna, PhD, Univ. of Notre Dame
This despite a long history that would suggest otherwise, perhaps most famously the story of the wisdom of king Solomon in I Kings 3: 16-28. Other historical documents, for example, the Other historical documents, for example, the Medieval Swedish Code of Guta, the 1816 Parish Church Council of Sweden and 1819 Midwifery regulations all recommend a separate sleep environment for infants.
Opponents of bed sharing cite a variety of potential problems including falls, overlaying. wedging or entrapment and thermal stress. The million-dollar question is whether this practice can it be done safely and/or by all?
“. . . such factors as maternal drug or alcohol use and inappropriate sleep conditions, such as a sofa (makes it) clear that there are two ends of a spectrum when it comes to co-sleeping and bed-sharing.” – McKenna
“SIDS/suffocation risk factors for co-sleeping include bed sharing not being the accustomed sleep arrangement, sofa sleeping, smoking parent, unsafe space between mattress and headboard or wall, prone sleeping, parent compromised by drugs or alcohol, overly heavy or fluffy bedding, sleeping with sibling or non-interested adult.” – Palmer

SUID Autopsy
An autopsy is essential in all SUID cases. This will include the following:
- External examination
- Radiographs
- Internal examination
- Microscopical studies
- Neuropathology
- Toxicology
- Microbiology
- Inborn errors of metabolism screen
- Other studies as indicated
What investigation and autopsy can prove . . .
- Myocarditis
- Congenital defects
- Rhabdomyoma
- Pneumonia
- Bronchiolitis
- Enterocolitis w/ electrolyte imbalance
- Cystic fibrosis
- Head trauma
- Congenital adrenal hypo- or hyperplasia
- Meningitis/encephalitis
- Vascular malformations of the brain
- Poisoning
- Suffocation/smothering
- Other asphyxia, e.g. overlaying, wedging
- Inherited abnormalities of cardiac electrical activity (LQTS)
Common, but non-diagnostic findings – these are described in a wide variety of infant deaths and are not specific for any given cause:
- Pulmonary congestion/edema/hemorrhage
- Petechiae
- Minimal to moderate terminal aspiration
- Small, focal, perivascular CNS hemorrhages
- Minimal evidence of aspiration – NOT a cause of death
- Non-diagnostic liver findings
- Old germinal matrix hemorrhage
Most common explained causes of sudden infant death
- Congenital heart disease
- CNS disease
- Infections
- Inborn errors of metabolism (MCAD)
- Growing promise of LQTS genetic screening
Asphyxia or Infanticide?
In certain cases, it is necessary to ask the question…these are some of the factors that must be taken into consideration.
- Wedging, overlaying
- Suffocation
- Fatal, occult child abuse
- Munchausen’s by Proxy (now known as “factitious disorder imposed on another”)
- Mimics of child abuse
SUID follow up
- Early notification of Bureau of Maternal and Child Health SIDS Counseling Services is routine in New Hampshire as is its equivalent in many other states
- Initial contact and resource referral immediately following autopsy
- Notification of parents of final autopsy results
- Long-term follow-up as dictated by individual case.
Conclusion
SUID is a devastating tragedy that is in some cases, preventable. This article by Dr Andrew has reviewed the state of understanding at this time. Families affected by this catastrophe should know there are resources and support available to them in all fifty states. The vast majority of families will by guided toward those resources, but in the unlikely event this has not happened, your primary care provider can assist.