It is estimated that between 1 and 2 million elderly Americans are abused annually, Elder Abuse is seen in all races and socioeconomic groups
The greying of America and the difficulty of identifying elder abuse.
Life expectancy has been increasing in America
- 1950 – 65
- 1980 – 72
- 2001 – 77
It is projected that by 2050 there will be 82 million older Americans (or 20% of population).
A much as 50% of elder abuse cases involve intimate partner or spouse. It is estimated that 80-90% are unreported, because of fear, shame or worries about abandonment.
Risk factors include poor health, social isolation, a family history of violence and perpetrator substance abuse.
Blunt impact injuries and asphyxia are the most common mechanisms of injury.
It is often difficult to identify elder abuse and to differentiate it from the normal aging process. In some cases, the cause of death may not be directly a result of abuse, but the abuse can be a significant contributing factor. Just because the official cause of death is accident or natural causes, does not necessarily absolve the abuser of responsibility.
The aging process can make it difficult to distinguish between natural aging and injury.
There is a marked variability in how people age. The interplay of degenerative changes and natural disease aggravates the lack of clarity.
Aging functionally impacts a person in many ways causing:
- Weakness
- Instability
- Immobility
- Deconditioning
- Sensory impairment
- Malnutrition
- Overall failure to thrive
For example, it often difficult to determine if purple discoloration of the skin is due to aging or injury as many seniors suffer from senile purpura and easy bruising.
The Typology of elder abuse can take several forms
- Physical
- Neglect
- Sexual
- Psychological
- Financial
- Violation of rights
- Medication abuse
Physical Abuse
Examples of physical abuse in seniors include contusions, lacerations and fractures, caused by hands, feet, objects, restraint and force feeding
Physical abuse can manifest as closed head injuries, skull and hip fractures, these are also commonly seen in falls.
Red flags for physical abuse include, multiple injuries of differing ages and implausible explanations for presenting injuries.
Asphyxia induced by external pressure about the neck or over the chest, restricting its normal motion may present petechiae (pinpoint spots of bleeding under the skin of the neck and face and in the lining of the eyes and mouth). Cartilaginous and/or bony injury of neck and upper airway obstruction may be identified at autopsy. High risk scenarios include the use of restraints, support straps, unsafe bed railings, neurodegenerative disease, dementia and ill-fitting dentures.
Example case studies
- Based on police information, an elderly woman found dead and with bruises over most of her body lives with her son, who is a career criminal and has a history of assault against his mother, typically for social security money.The autopsy showed a duodenal ulcer with peritonitis and cirrhosis of liver.Further investigation found a reliable witness report that the woman fell down three concrete steps at a package store, after purchasing liquor, four days before death.As a result no case could be made against the son.
- 84-year-old male with multiple medical problems and a history of frequent falls was found dead in bed, Police report a hstory of domestic violence in the home. His spouse stated the decedent had fallen earlier in the day, and that later he was holding a pillow over his head saying he wanted to die.When found dead, his wife called a funeral home for pick-up, then called local fire station.
Police and the funeral home arrived simultaneously. The case was referred to the medical examiner for evaluation. Autopsy revealed an acute subdural hematoma with no external or occult injuries, old or new. Investigation corroborated the history.Toxicology – carbamazepine (anticonvulsant) and warfarin (blood thinner).
Cause of death was determined to be blunt impact injury of the head with subdural hematoma, due to a fall from standing height. Contributing to death was the anticoagulation therapy. The manner of death was an accident.
Neglect
Neglect as a form of elder abuse can be active or passive and can include nutrition or hydration, clothing/hygiene, shelter and social stimulation. Another form of this kind of abuse is allowing self-neglect.
Example case study
65-year-old female with neurological issues due to a treated brain tumor and collateral damage from radiation treatment. She was found dead at home by her husband 20 minutes after seeing her alive.
The primary care physician in a neighboring state had filed an Elder Neglect Complaint and was “uncomfortable” certifying death, stating, she feared for decedent’s safety and alluding to “several subdural hematomas”
A deeper look at her history
- Grade 2 astrocytoma of hypothalamus treated in 1999
- Sequelae – panhypopituitarism, seizure disorder, dementia, hyperprolactinemia, urinary incontinence, gait instability
- Co-morbidities – “vasculopathy” with stroke, hyperlipidemia
- Would periodically become non-verbal and remain in bed for several days
The decedent had had frequent falls with fractures, including falling while walking her dogs. Three weeks prior to her death, he sustained a comminuted fracture of her right olecranon (elbow). Additional extremity fractures were incurred in another fall while walking her dogs, along with a scalp laceration. Radiographical studies revealed L1 and L3 fractures (CT) and anterolateral fractures of rib 5-7 (plain films).
Findings at autopsy, in addition to corroboration of clinically identified injuries, included hypertensive changes of heart and kidneys, centrilobular emphysema, renolithiasis with right hydronephrosis and generalized osteopenia.
Brain examination revealed no residual or recurrent tumor with reactive gliosis of temporal lobes, sings of remote subdural hematoma and chronic arteriosclerotic changes.
Vitreous electrolytes showed a non-diagnostic pattern and toxicology revealed the presence of acetaminophen, carbamazepine and levetiracetam.
Conclusion
Police investigation does did not reveal information of concern. Death was certified as natural caused by complications of the grade 2 astrocytoma
Pressure (Decubitus) Ulcers also known as bed sores
Prolonged immobility, particularly in the bed-ridden state may lead to pressure ulcers. These result from pressure at a bony site, which causes obstruction of capillary flow resulting in soft tissue necrosis
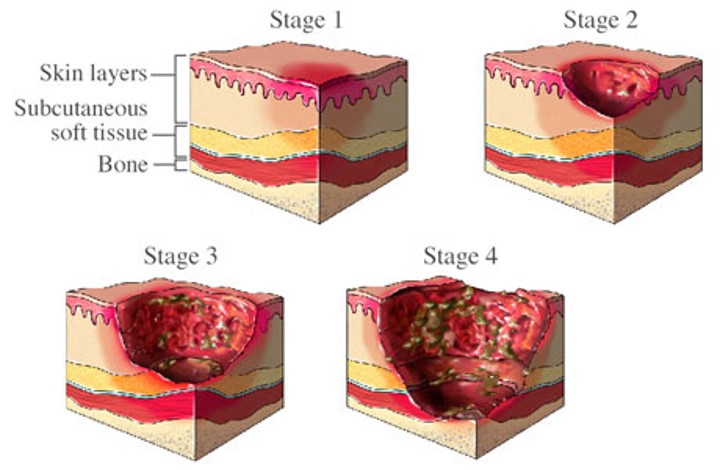
The most common sites for pressure ulcers are the scapulae, posterior spinous processes, sacrum, occipital scalp and heels
Changes can develop within 2-6 hours. Risk factors include, diabetes, arteriosclerosis, sepsis and hypotension from causes other than sepsis. Pressure ulcers affect
- 10% 0f hospitalized patients
- 20% of nursing home patients
- 30% of those with spinal cord injuries
While not necessarily indicative of neglect, red flags include multiple ulcers and ulcers extending to the bone.
Example case study
An 88-year-old female living at home with assistance of a granddaughter, presented to ED with a 2-3 day history of lethargy and anorexia per the granddaughter. Rectal temperature 87 degrees F. A sacral decubitus ulcer was infested with maggots and her body was infested with bedbugs. Additionally, there was a pressure sore of the right heel and skin tears of the forearms. 12 inches of severely matted hair had to be cut for hygiene purposes.
Stool culture was positive culture for C. difficile. There was also a urinary tract infection and marked dehydration. A neglect report was filed with Bureau of Elderly and Adult Services. BEAS which already had a neglect/financial abuse case open.
The woman died after nine-day hospitalization and the granddaughter requested immediate release to funeral home and objected to autopsy
Autopsy revealed hypertensive changes of heart and kidney, diverticulosis and uterine leiomyomas. Toxicology revealed acetone 12 mg/dL, donepezil 61 ng/mL and an elevated level of morphine at 670 ng/mL.
While the cause and manner of death were certified as natural, neglect’s role in hastening death resulted in charges against the granddaughter.
Sexual Abuse
This type of abuse may or may not leave grossly evident injury. A standard sexual assault kit is recommended when indicated.
There are issues to be considered as explanations for the appearance of injury or as factors that could aggravate injury due to abuse, for example lichen sclerosis et atrophicus (a skin disease of unknown cause, commonly appearing as whitish patches on the genitals), Another potential cause of friable, easily torn mucosa is chronic incontinence
Psychological Abuse
 This can include threats of abandonment, institutionalization and physical harm. Also, humiliation and verbal aggression
This can include threats of abandonment, institutionalization and physical harm. Also, humiliation and verbal aggression
Elder Abuse – Financial Abuse
This can include the misuse of assets such as the spending of savings and the withholding of basic needs and the diversion of benefits. Outright theft of money, property and personal items and coercion to deprive the senior of their assets are additional forms of financial abuse.
Financial abuse is frequently accompanied by other forms of abuse
Violation of Rights
This may include abandonment, no voice in decision-making and denial of privacy
Medication Abuse
This may be by the withholding of medication or providing the wrong medication and/or wrong dose. Intentional sedation with opioids and/or anxiolytics has been documented in numerous cases.
Potentially mitigating/aggravating contexts to be considered included altered metabolism, decreased organ reserves, anticoagulation and drug interactions (those over 65 take an average of 7 medications).
Example case study
An 80-year-old male with hypertension, arteriosclerosis, dementia and atrial fibrillation died at home in presence of his wife and his long-time home health aide. He had initial signs of dementia as early as 2008. He sustained multiple severe injuries in motorcycle crash in 2012 with accelerated deterioration in cognitive status.
The case reported to the medical examiner and jurisdiction was declined.
A nephew from California called with allegations of abuse, neglect and overmedication, and the medical examiner then accepted jurisdiction. Autopsy revealed no externally evident signs of abuse or neglect. Three months of Home Health and Hospice notes appeared in order and the primary physician had no concerns. The police investigation did not substantiate the nephew’s allegations.
Autopsy showed
- Fibrinopurulent bronchopneumonia
- Hypertensive changes of heart and kidneys
- Benign enlargement of the prostate gland
- Diverticulosis
- Vitreous: Na 160 mmol/L, VUN 54 mg/dL, creatinine 1.6 mg/ dL
- Neuropathology:
- Old lacunar infarction
- Alzheimer-type changes of hippocampus
- Toxicology: morphine 9.4 ng/mL
Conclusion
Cause of Death:
Acute, fibrinopurulent bronchopneumonia due to dementia consistent with Alzheimer’s disease. Remote traumatic brain injury
Manner of Death: Accident
Case Investigation
Because of the effects of aging, the diagnosis of elder abuse requires a high index of suspicion in many ways similar to child abuse.
Thorough documentation of injuries (new vs old, evident vs occult) is crucial. Injuries must be placed in their proper context of natural disease/co-morbidities.
One form of abuse may open the door to the discovery of others.
Interagency cooperation in the context of a well-coordinated public health and safety response may mean the difference between burying or cremating a person who has died naturally of has been the victim of criminal abuse or neglect.
Formation of elder abuse death review teams, modeled largely on pre-existing child and domestic violence fatality teams with slight modifications is becoming more routine in the US.

